We've been talking about smell loss and the best ways to measure for it at PREDICT-PD recently. Hyposmia or anosmia is the most common non-motor symptom in Parkinsons patients and can be present many years before diagnosis. We can test smell formally with various tests, the most widely used being the University of Pennsylvania smell test (UPSIT), which tests 40 common odours including coffee, chocolate and strawberries.
It is proposed that this symptom indicates that the neurodegenerative process in PD starts outside of the brain itself and perhaps in the peripheral nervous system but there are few studies which directly address the reasons for smell loss and the underlying mechanisms. MRI is a good candidate for this - recent studies have used high resolution MRI to look more closely at problems in the visual systems in Parkinsons and the study below, by researchers in Iran and Switzerland uses MRI to ask whether there are imaging findings associated with smell loss.
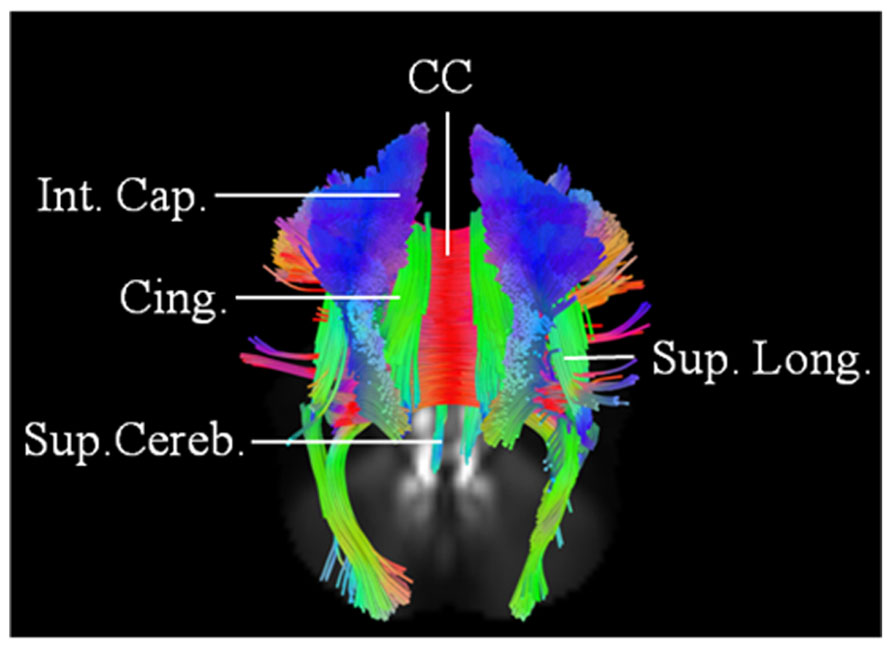
They use the large cohort study PPMI, which has recruited patients with early Parkinsons and used a technique called connectometry, which allows analysis of white matter tracts, the main pathways in the brain. A number of pathways were found to be significantly different between patients with different levels of smell loss. Tracts involving the limbic system, which mediates emotion, memory and some aspects of behaviour were particularly sensitive for early smell loss. This is an interesting finding as these areas are not traditionally associated with Parkinsons.
This is early work but as new techniques for MRI analysis continue to be developed and our ability to image these previously unseen parts of the brain develops we are getting a fuller picture of why these symptoms develop, how to measure them and fundamentally, how to prevent their degeneration.
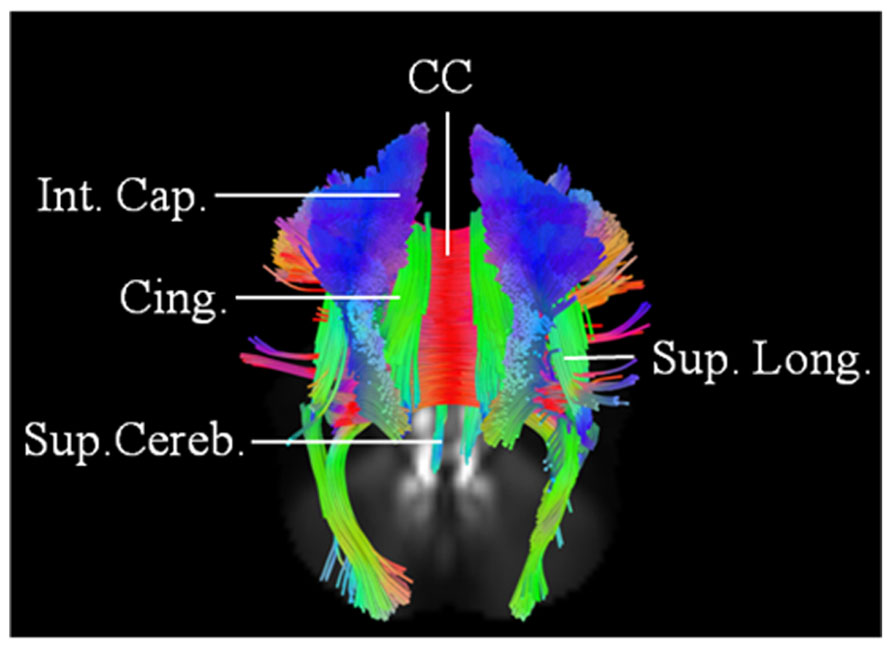 |
| An Example of the Connectometry approach, showing tracts in the brain |
Brain Imaging Behav. 2017 Nov 13. doi: 10.1007/s11682-017-9781-0. [Epub ahead of print]
Exploring white matter microstructure and olfaction dysfunction in early parkinson disease: diffusion MRI reveals new insight.
Sobhani S, Rahmani F, Aarabi MH, Sadr AV.
Olfaction dysfunction is considered as a robust marker of prodromal Parkinson disease (PD). Measurement of olfaction function as a screening test is unsatisfactory due to long lead time interval and low specificity for detection of PD. Use of imaging markers might yield more accurate predictive values and provide bases for combined use of imaging and clinical markers for early PD. Diffusion MRI connectometry was conducted on 85 de novo PD patients in and 36 healthy controls to find: first, white matter tracts with significant difference in quantitative anisotropy between PD groups with various degrees of olfaction dysfunction and second, second fibers with correlation with University of Pennsylvania Smell Identification Test (UPSIT) score in each group using a multiple regression analysis considering age, sex, GDS and MoCA score. Local connectomes were determined in seven of all the possible comparisons, correcting for false discovery rate (FDR). PD patients with anosmia and normal olfaction had the highest number of fibers with decreased connectivity in left inferior longitudinal fasciculus, bilateral fornix, bilateral middle cerebellar peduncle (MCP), bilateral cingulum, bilateral corticospinal tract (CST) and body, genu and splenium of corpus callosum (CC) (FDR = 0.0013). In multiple regression analysis, connectivity in the body, genu and splenium of CC and bilateral fornix had significant negative correlation (FDR between 0.019 and 0.083), and bilateral cingulum and MCP had significant positive correlation (FDR between 0.022 and 0.092) with UPSIT score. White matter connectivity in healthy controls could not be predicted by UPSIT score using the same model. The results of this study provide compelling evidence that microstructural degenerative changes in these areas underlie the clinical phenotype of prodromal olfaction dysfunction in PD and that diffusion parameters of these areas might be able to serve as signature markers for early detection of PD. This is the first report that confirms a discriminative role for UPSIT score in identifying PD specific changes in white matter microstructure. Our results open a window to identify microstructural signatures of prodromal PD in white matter.
It is highly relevant to discussion on the route of origin and progress in PD to realise that the loss of the sense of smell (along with other symptoms)can be reversed with the use of food additives taken daily as I can personaly vouch for. It appears to be the neuronal connections to the olfactory epithelial sensor cells that are faulty and the lack of connection can be restored. This indicates the possibility of restoration of neurons throughout the system.
ReplyDelete