Happy new year! I hope you've had a relaxing break and taken the time to catch up on some all-important sleep (see http://predictpd.blogspot.co.uk/search?q=sleep). I'm continuing this year to look at cognitive function in participants in the PREDICT-PD study and we have been talking about using imaging as a tool to understand better the reasons that cognition may deteriorate in the early stages or even before Parkinson's develops. One of the suggestions is that there may also be Alzheimers-type pathology in these patients.
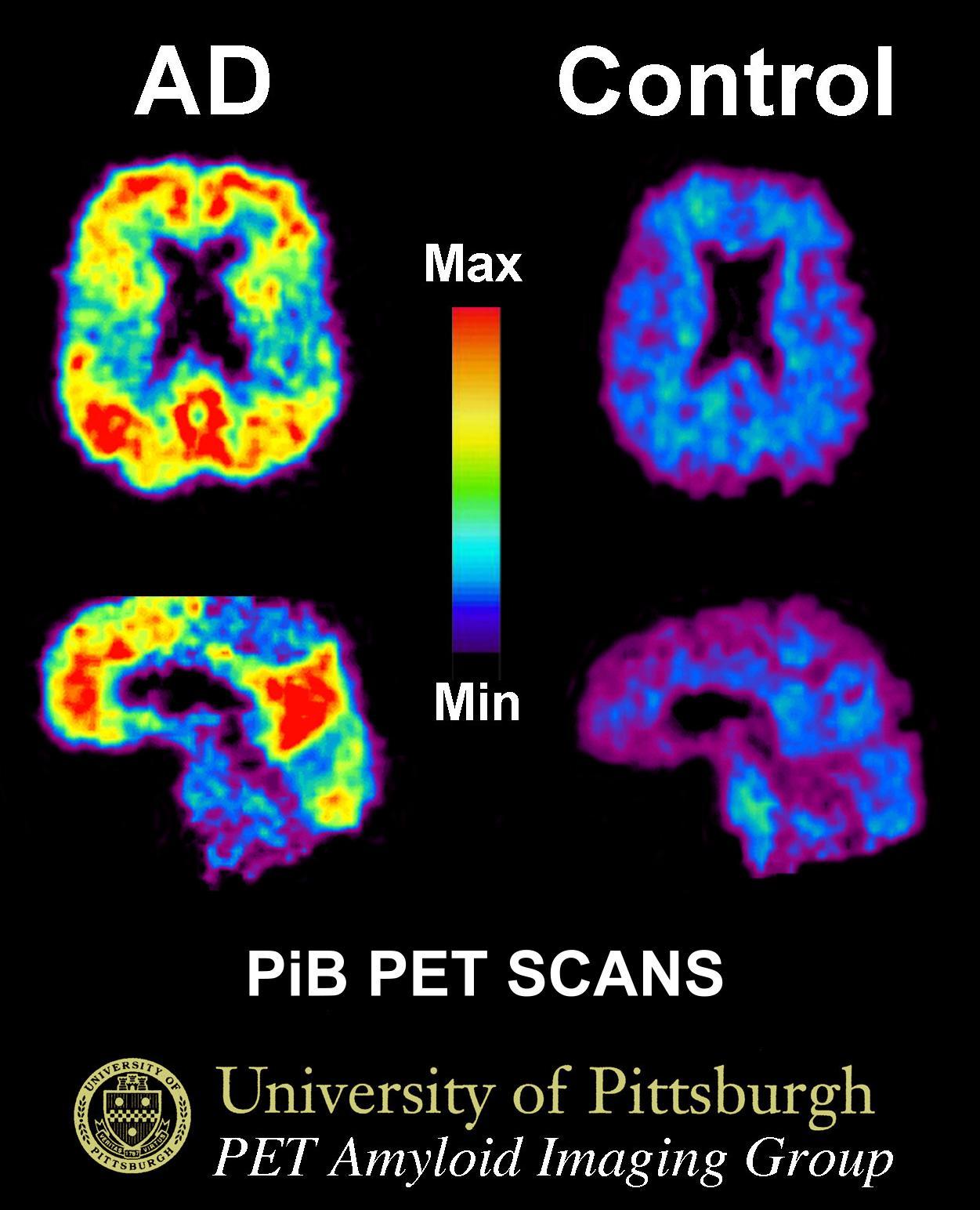
This study, from a team based in the states, used three different types of imaging as well as cognitive tests to ask the question "Do the brains of people with Parkinson's who have declining cognition look similar to people with Alzheimer's?" We know that in Alzheimer's there is build up of a protein called amyloid outside cells and a protein called tau inside cells. We now have techniques that use nuclear tracers to label both amyloid and tau in the brain - this signal can be detected using a PET scan so that we can build up a picture of protein deposition in the brain. In advanced Alzheimers disease, amyloid "lights up" throughout the brain - shown in red in the image - indicating the areas with abnormal deposits of the protein.
In this study, where 30 patients with Parkinson's disease and 49 healthy participants underwent scanning, they didn't find any differences in scan results between people with Parkinson's disease who had normal cogntive function, those who had poorer cognitive function. In fact, all the scans looked similar to healthy participants.
This is an important finding, but we should take some caution with the interpretation that cognitive decline in Parkinson's has nothing to do with Alzheimer's-like pathology. Previous studies have shown an association between cognitive decline over time and amyloid - which this cross-sectional study was unable to address. The level of cognitive function in the study was generally high (on correspondence with the author only 1/29 were cognitively impaired on a standard screening test which is far lower than in other studies) and the criteria for classifying cognitive impairment was relatively lax so may have included participants with borderline cognition not just those at the more severe end of the spectrum. More work needs to be done in this area with larger numbers of patients who have significant cognitive problems before we will have a clear answer.
-Anna
https://www.ncbi.nlm.nih.gov/pubmed/29228071
JAMA Neurol. 2017 Dec 11. doi: 10.1001/jamaneurol.2017.3713. [Epub ahead of print]
Associations Between Tau, β-Amyloid, and Cognition in Parkinson Disease.
Winer JR, Maass A, Pressman P, Stiver J, Schonhaut DR, Baker SL, Kramer J, Rabinovici GD, Jagust WJ.
Abstract
Importance:
Multiple disease processes are associated with cognitive impairment in Parkinson disease (PD), including Lewy bodies, cerebrovascular disease, and Alzheimer disease. It remains unknown whether tau pathology relates to cognition in patients with PD without dementia.
Objective:
To compare tau aggregation in patients with PD who are cognitively normal (PD-CN), patients with PD with mild cognitive impairment (PD-MCI), and healthy control participants, and evaluate the relationships between β-amyloid (Aβ), tau, and cognition in patients with PD who did not have dementia.
Design, Setting, and Participants:
This cross-sectional study recruited 30 patients with Parkinson disease (15 with PD-CN and 15 with PD-MCI) from a tertiary care medical center and research institutions from July 2015 through October 2016. One patient with PD-MCI did not receive a magnetic resonance imaging scan and thus was excluded from all analyses; 29 patients with PD were included in the present study. Participants underwent tau positron emission tomographic (PET) scanning with fluorine 18-labeled AV-1451, Aβ PET scanning with carbon 11-labeled Pittsburgh compound B, magnetic resonance imaging, cognitive testing, and neurologic evaluation. Imaging measures were compared with 49 healthy control participants.
Main Outcomes and Measures:
Outcomes were tau PET measurements of groups of patients with PD-CN and PD-MCI. We hypothesized that tau aggregation across groups would be related to age and Aβ status.
Results:
Of the 78 participants, 47 (60%) were female, and the mean (SD) age was 71.1 (6.6) years. Six patients with PD (21%) were Aβ-positive, of whom 1 was mildly cognitively impaired; 23 were Aβ-negative (79%). (Of the 49 healthy controls, 25 were Aβ-negative and 24 Aβ-positive.) Voxelwise contrasts of whole-brain tau PET uptake between patients with PD-CN and patients with PD-MCI, and additionally between all patients with PD and Aβ-negative controls, did not reveal significant differences. Tau PET binding did not differ between patients with PD-MCI and PD-CN in brain regions reflecting Alzheimer disease Braak stages 1/2, 3/4, or 5/6, and did not differ from Aβ-negative healthy older adults. Mean (SD) tau PET binding was significantly elevated in Aβ-positive patients with PD relative to Aβ-negative patients with PD within brain regions reflecting Alzheimer disease Braak stage 3/4 (1.22 [0.07] vs 1.14 [0.07]; P = .03) and Braak stage 5/6 (1.20 [0.07] vs 1.11 [0.08]; P = .02).
Conclusions and Relevance:
These findings suggest that patterns of cortical Aβ and tau do not differ in people with PD-CN, people with PD-MCI, and healthy older adults. Age, Aβ, and tau do not differentiate patients with PD-CN and PD-MCI. Tau deposition is related to Aβ status and age in both people with PD and healthy older adults. Cognitive deficits in people with PD without dementia do not appear to reflect measureable Alzheimer disease.
No comments:
Post a Comment