Predictive medicine is becoming increasingly complex, with predictive models which incorporate both clinical information and a huge range of biomarkers. Biomarkers commonly used in neurodegenerative disease include molecules in bodily fluids such as saliva, blood and spinal fluid and genetic data from these sources, scans for both structural aspects of the brain and molecular studies which can quantify the amount of protein build up in the brain. These biomarkers vary in how invasive and risky they are to collect and while they may help us understand the disease process, many people are uncomfortable with going through an invasive procedure such as lumbar puncture.
The basis of the current PREDICT-PD model is to use participant survey to collect clinical information to predict risk. The study below, from a team in Quebec, also uses a clinical approach. They looked at a group of people with Parkinsons' disease and used an 8 item scoring scale including age, evidence of cognitive impairment at baseline, motor features such as freezing or falls, drop in blood pressure on standing and features of rapid eye movement sleep behaviour disorder.
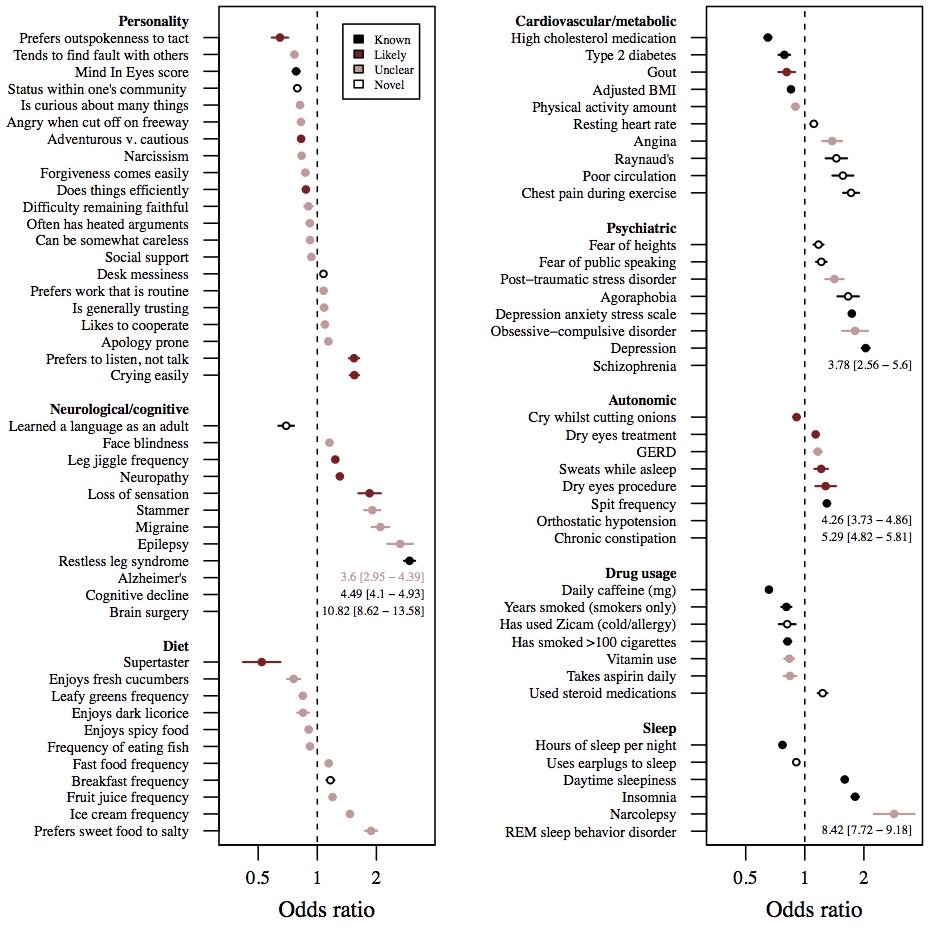
Interestingly, the predictive value of this model seems to be as good as studies which include biomarker values such as amyloid protein levels in the spinal fluid. Biomarker studies in this area will continue to be important, especially as they hold the hope of elucidating the molecular processes which can be interrupted to disrupt the progression of disease. But this is a good reminder of the power that can be harnessed from information which is available simply by asking questions of and examining our patients.
-Anna
Office-Based Screening for Dementia in Parkinson Disease: The Montreal Parkinson Risk of Dementia Scale in 4 Longitudinal Cohorts.
IMPORTANCE:
Parkinson disease dementia dramatically increases mortality rates, patient expenditures, hospitalization risk, and caregiver burden. Currently, predicting Parkinson disease dementia risk is difficult, particularly in an office-based setting, without extensive biomarker testing.
OBJECTIVE:
To appraise the predictive validity of the Montreal Parkinson Risk of Dementia Scale, an office-based screening tool consisting of 8 items that are simply assessed.
DESIGN, SETTING, AND PARTICIPANTS:
This multicenter study (Montreal, Canada; Tottori, Japan; and Parkinson Progression Markers Initiative sites) used 4 diverse Parkinson disease cohorts with a prospective 4.4-year follow-up. A total of 717 patients with Parkinson disease were recruited between May 2005 and June 2016. Of these, 607 were dementia-free at baseline and followed-up for 1 year or more and so were included. The association of individual baseline scale variables with eventual dementia risk was calculated. Participants were then randomly split into cohorts to investigate weighting and determine the scale's optimal cutoff point. Receiver operating characteristic curves were calculated and correlations with selected biomarkers were investigated.
MAIN OUTCOMES AND MEASURES:
Dementia, as defined by Movement Disorder Society level I criteria.
RESULTS:
Of the 607 patients (mean [SD] age, 63.4 [10.1]; 376 men [62%]), 70 (11.5%) converted to dementia. All 8 items of the Montreal Parkinson Risk of Dementia Scale independently predicted dementia development at the 5% significance level. The annual conversion rate to dementia in the high-risk group (score, >5) was 14.9% compared with 5.8% in the intermediate group (score, 4-5) and 0.6% in the low-risk group (score, 0-3). The weighting procedure conferred no significant advantage. Overall predictive validity by the area under the receiver operating characteristic curve was 0.877 (95% CI, 0.829-0.924) across all cohorts. A cutoff of 4 or greater yielded a sensitivity of 77.1% (95% CI, 65.6-86.3) and a specificity of 87.2% (95% CI, 84.1-89.9), with a positive predictive value (as of 4.4 years) of 43.90% (95% CI, 37.76-50.24) and a negative predictive value of 96.70% (95% CI, 95.01-97.85). Positive and negative likelihood ratios were 5.94 (95% CI, 4.08-8.65) and 0.26 (95% CI, 0.17-0.40), respectively. Scale results correlated with markers of Alzheimer pathology and neuropsychological test results.
CONCLUSIONS AND RELEVANCE:
Despite its simplicity, the Montreal Parkinson Risk of Dementia Scale demonstrated predictive validity equal or greater to previously described algorithms using biomarker assessments. Future studies using head-to-head comparisons or refinement of weighting would be of interest.